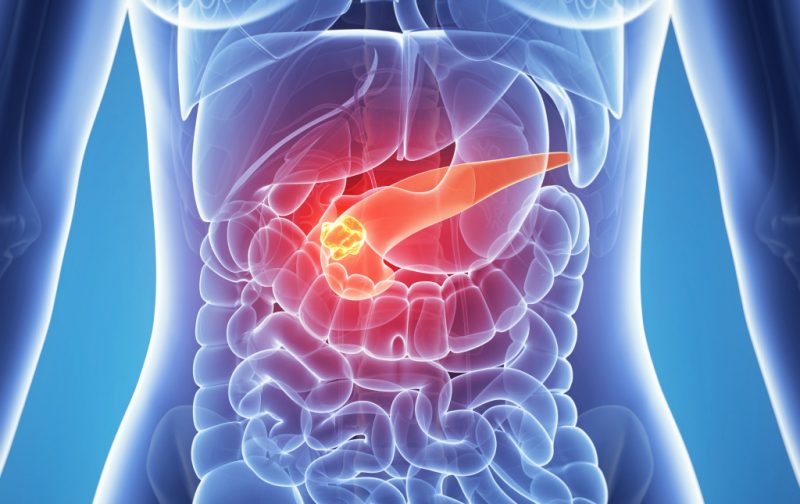
The health of our gastrointestinal tract depends on the coordinated work of all organs of the digestive system. Pancreatic juice, produced during digestion, helps break down substances that come with food. In chronic pancreatitis, the fluid begins to act not in the duodenum, but directly in the pancreas, which leads to the development of serious pathologies.
Material Content:
Causes of Chronic Pancreatitis
In the inflammatory process, gland cells die, and at more advanced stages, pancreatic necrosis can develop, which poses a serious threat to human life.
The main causes of chronic pancreatitis are:
- Excessive alcohol consumption. In almost 50% of patients, this disease developed against the background of alcohol abuse. Under the influence of alcohol in the pancreas, the number of enzymes produced increases. At the same time, the organ significantly slows down its functions, as a result of which pancreatic juice activates its action inside the gland, before it reaches the intestine. In addition, ducts are spasmodic, through which the produced fluid enters the duodenum. In the end, the pancreas begins to digest itself.
- Improper nutrition. If the daily diet is dominated by fatty, spicy or salty foods.Excessive overeating leads to negative consequences, when a person eats nothing during the day and eats a large portion on an empty stomach before going to bed.
- The presence of stones in the gallbladder. If the diagram shows the location of the channels of the gastrointestinal tract, then you can see that the ducts of the gallbladder and pancreas in a certain area are connected, forming a single duct. A stone located in the bile duct is able to block access to the duodenum, thus provoking a delay in enzymes.
- Infectious diseases. Chronic pancreatitis can develop amid complications caused by hepatitis B and C or mumps virus.
Symptoms and signs of the disease
The main bell, indicating the presence of an inflammatory process in the pancreas, is a pulling pain in the abdomen, radiating to the dorsal region. Often, discomfort occurs an hour after eating. There are cases when the pain syndrome manifests itself after a few days. This usually happens after alcohol abuse.
In addition to periodically occurring in the abdominal pain, the following symptoms of chronic pancreatitis are distinguished:
- indigestion, accompanied by nausea and vomiting reflex;
- loose stools;
- poor appetite;
- chronic flatulence.
Important! The signs of the disease are constantly changing. The danger of the chronic form is that the symptoms characteristic of this ailment may subside for a long period of time or may not appear at all.
Exacerbation of chronic pancreatitis
During the period of exacerbation, the patient has a white coating on the tongue, rapid weight loss, as well as symptoms of vitamin deficiency, such as “seizures” in the corners of the oral cavity, dehydration of the skin, hair loss, etc. Complications lead to severe pain during abdominal palpation.
In addition, the advanced stage of the disease provokes the development of a Gray-Turner symptom, in which hemorrhages form in the superficial tissues of the abdomen. On palpation, the doctor can detect a dense formation in the patient caused by an enlargement of the pancreas.
Very often, exacerbation of chronic pancreatitis is observed as a result of following an improper diet. The patient rapidly loses weight, his activity decreases, problems with sleep are observed, which, ultimately, leads to the emergence of deep depression.
Diagnostic measures
The most difficult to detect inflammation of the pancreas in the early stages of the disease. In order to correctly diagnose the disease, the gastroenterologist conducts a number of clinical studies that can detect pancreatitis even in the initial stages.
- General blood analysis. Specialists determine the level of leukocytes, the erythrocyte sedimentation rate (ESR). These studies help to detect inflammatory processes that occur in the gastrointestinal tract.
- Blood biochemistry. Thanks to this diagnostic method, it is possible to obtain information about metabolism, to determine the level of enzymes in the pancreas, and also to determine the amount of glucose in the blood.
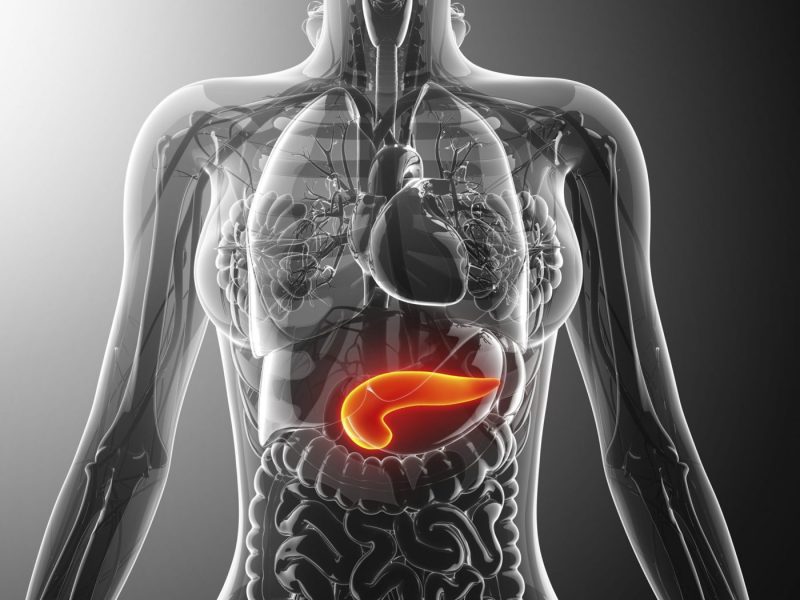
- Ultrasound examination of the abdominal organs. The doctor visually assesses the state of the digestive system, determines the size of the pancreas and its structure.
- Roentgenography. This technique is designed to diagnose the biliary tract.
- Analysis of urine. An increased level of amylase signals the presence of an inflammatory process (most often observed in acute form of pancreatitis).
Pancreatic Disease Treatment
Treatment of chronic pancreatitis is aimed at restoring all the functions of the abdominal organs.At the time of the exacerbation of the disease, adults are prescribed a strict diet, and in some cases it is recommended that they completely refrain from eating food for several days. Due to this, the pancreas temporarily stops its work and ceases to secrete pancreatic juice.
Drug treatment
Medicines prescribed by the attending physician should perform a number of the following functions:
- Relieve pain. In cases where the disease is accompanied by severe pain, the patient is prescribed medications, the action of which is aimed at eliminating spasms. A pronounced effect is possessed by No-spa, Atropine, Novocaine or Promedol.
Important! In chronic pancreatitis, non-steroidal anti-inflammatory drugs such as Aspirin or Ketanov should not be used.
- Reduce the production of enzymes. For this, medications are prescribed that suppress the secretion of gastric acid. These include omeprazole capsules.
- To have an antibacterial effect. In order to prevent the development of pathogenic microorganisms, antibiotics such as Amoxil are prescribed.
- Restore water-electrolyte balance. For this, the patient is given droppers using physiological solutions.
Traditional medicine recipes
- Oat Kissel. The washed oats are poured with purified water, after which the mixture is left to infuse for two days. Then the cereal is dried and ground to a powder state. The finished ingredient is added to water. The resulting mixture is boiled for several minutes, and then the jelly is insisted for another half hour. Means based on oats are drunk exclusively fresh.
- Potato juice. The potato juice obtained using a juicer is drunk daily 15 minutes before a meal. For best results, juice is drunk twice a day: morning and evening.
Surgical intervention
In medicine, direct and indirect methods of treating pancreatitis are distinguished. Indirect methods include operations on the bile ducts, as well as surgical interventions on the abdominal organs. Among the direct methods of treatment, internal drainage of the cyst, removal of the head of the pancreas and gallstones are distinguished.
Surgical intervention is prescribed by your doctor if:
- there is an advanced stage of the disease in which obstructive jaundice is diagnosed;
- pronounced pain syndrome that does not stop even under the influence of medications;
- a cyst is formed.
Diet for chronic pancreatitis
Strict adherence to all necessary nutritional restrictions will prevent the subsequent exacerbation of pancreatitis. Gastroenterologists recommend that their patients exclude from the diet fatty, sweet, salty and spicy foods that provoke excessive production of pancreatic juice.
Patients should not eat smoked products, canned food, sausages, as well as hot spices, chocolate and spirits. In addition, food should be taken in small amounts 4-5 times a day to minimize exposure to the pancreas.
Complications and prognosis
The advanced stage of the disease can cause various infectious and inflammatory complications, such as purulent cholangitis and ligamentitis, as well as acute septic conditions caused by the development of bacteria.
The most common complication is cholestasis, in which there is a rapid decrease in the production of bile secretion. Stagnation of bile, in turn, leads to the formation of stones in the gallbladder and contributes to the development of liver failure.
Important! Timely diagnosis and proper treatment of pancreatitis will help to avoid subsequent complications of the chronic form of the disease.
Prevention
To avoid exacerbation of chronic pancreatitis, the patient must be systematically (at least 2 times a year) examined in a specialized institution.It will only be possible to reduce the risk of complications if the patient unconditionally follows all the recommendations of the gastroenterologist.
Basic preventive measures:
- compliance with all nutrition rules, the exclusion of junk food and fast food;
- sufficient water consumption;
- inclusion in the diet of products enriched with healthy vitamins.
And remember that the most harmful effect on the state of the pancreas is the abuse of bad habits. In order for the disease to be in the lull stage for as long as possible, it is necessary to completely abandon the use of alcoholic beverages and tobacco products.