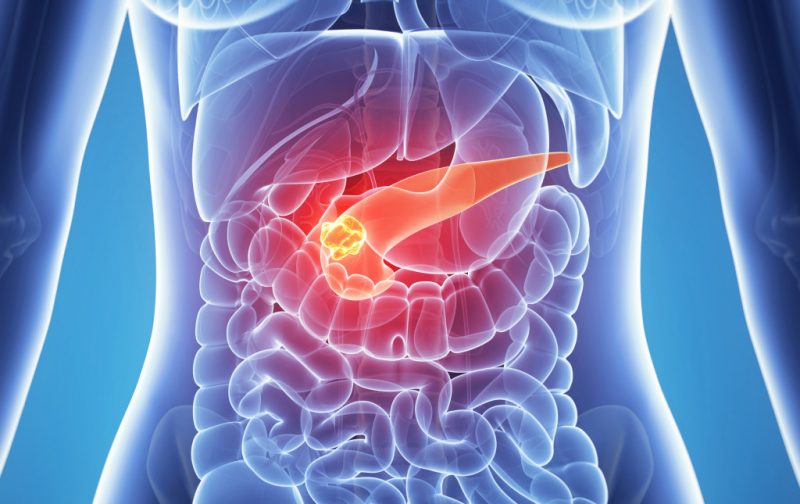
Malfunctions of the pancreas’s functionality are often accompanied by severe painful sensations and sufficiently complicate the usual course of the patient’s daily life. Pancreatitis is recognized as one of the most common diseases of this type. How to recognize and how to treat pancreatitis, are there effective measures to prevent this disease?
Material Content:
Causes and symptoms of pancreatitis
The causes of pancreatitis can differ depending on the gender and age of the patient.
Causes of pancreatitis in men:
- Frequent drinking, causing "alcoholic" pancreatitis.
- Failure to comply with the principles of a healthy diet, abuse of fatty and salty foods.
- Ignoring the typical symptoms of pathology and exacerbations, the result of which often becomes pancreatitis in a neglected form.
Reasons for the appearance of female pancreatitis:
- Gallstone disease (capable of causing cholecystitis along with pancreatitis).
- Hormonal disruptions that provoke inflammation in the pancreas (menopause, the period of gestation, the course of oral contraceptives).
- Starvation, tight diets.
Causes of pancreatitis in children:
- Injuries or postoperative consequences resulting in damage to the tissues / ducts of the gland.
- Hereditary predisposition to food allergies, chronic inflammatory processes, excessive production of gastric juice.
Secondary pancreatitis is able to develop as a symptom of various pathologies, and as a result of injuries of the peritoneal organs, previous operations, etc.
In addition, this condition may be due to the following pathologies:
- non-infectious hepatitis;
- gastritis;
- cirrhosis of the liver;
- biliary dyskinesia;
- intestinal infections.
Some statistics! In approximately 30% of cases, it is not possible to establish the exact cause of the development of pancreatitis.
It happens that a person does not suspect the presence of pancreatitis.
You should seek medical help, noting the following symptoms of the early stage of the disease:
- frequent heartburn, belching;
- persistent feeling of heaviness in the stomach;
- flatulence;
- increase in body temperature;
- nausea, vomiting, diarrhea.
 One or more of these symptoms can become a companion of the inflammatory process in the pancreas.
One or more of these symptoms can become a companion of the inflammatory process in the pancreas.
Chronic pancreatic disease
Chronic pancreatitis in its manifestations is extremely similar to its acute form, but its symptoms are often lightened. Sometimes the chronic form is observed if the patient abuses fatty, spicy foods, alcohol.
Sometimes patients have diarrhea, lack of appetite, bloating. In addition, this form of the disease is distinguished by belching and excessive salivation. At the same time, so much saliva can accumulate that the patient will have to constantly spit it.
In some cases, against the background of chronic pancreatitis, diabetes, jaundice, and nervous disorders can occur - a person becomes agitated and irritable, sometimes falls into depression.
Chronic pathology can occur in two forms:
- At the initial stage, the symptoms of the disease are relatively mild. The disease can be felt for many years, but do not seriously disturb the patient.
- Exacerbation of chronic pancreatitis is often inextricably linked to the patient's nutritional characteristics. Symptoms of the disease begin to bother the patient more often.
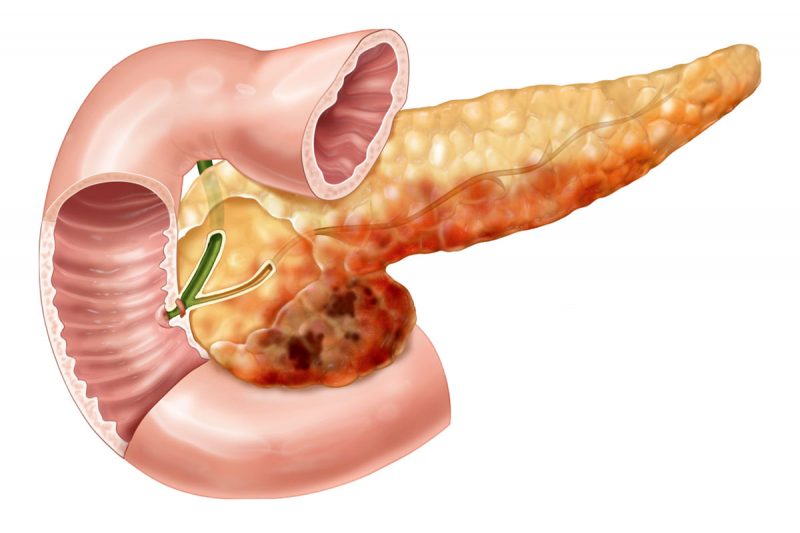
Signs of the chronic form of the disease and the lack of timely therapy that are neglected can provoke pancreatic cancer in the future.
Acute pancreatitis
The main symptom of acute pancreatitis in adults and children is considered to be pain in the area below the stomach in the left hypochondrium. Sometimes unpleasant sensations can be localized in the shoulder or kidney area on the left. Therefore, the signs of acute pancreatitis are often confused with heart pathologies.
 In addition to severe pain that accompanies an attack of pancreatitis and often causes shock, the patient may suffer from vomiting, diarrhea, or, conversely, constipation. The abdomen will be swollen and hard. An additional sign is a sharp jump in pressure indicators, accompanied by heart palpitations and shortness of breath.
In addition to severe pain that accompanies an attack of pancreatitis and often causes shock, the patient may suffer from vomiting, diarrhea, or, conversely, constipation. The abdomen will be swollen and hard. An additional sign is a sharp jump in pressure indicators, accompanied by heart palpitations and shortness of breath.
Sometimes pathology can provoke bluish spots in the lower back and navel. In addition, such a disease can be an impetus for the development of jaundice or renal failure.
Children during an attack can experience severe pain under the pit of the stomach or in the lumbar region, accompanied by hyperthermia and blanching or yellowing of the skin. The sclera of the eyes can also take an atypical yellow tint. Vomiting almost does not bring relief, in the last traces of bile are tracked.
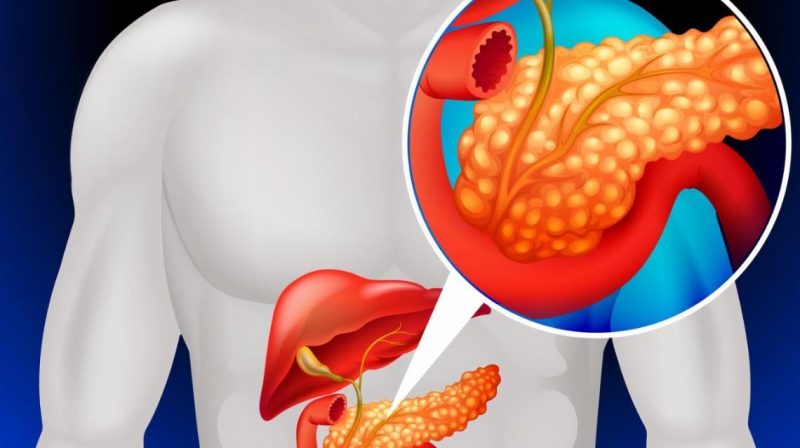
Diagnostics
In the process of diagnosing pancreatitis, a gastroenterologist uses instrumental and laboratory research methods:
- General blood test (detection of inflammation).
- Biochemical blood test (determination of the level of enzymes). In patients suffering from pancreatitis, the level of alpha-amylase exceeds the norm by 10 times.
- Blood test for sugar. Conducted to track glucose readings.
- Analysis of urine. Traces of amylase in urine are often considered precursors of acute pancreatitis.
- X-ray of the peritoneal organs.
- CT scan.
- Coprogram (feces analysis) .https: //www.youtube.com/watch? V = PY-jBJU1hj8
In some cases, the patient is recommended by ultrasound of the peritoneal organs to track changes in the gland. Using this diagnostic method, you can track typical manifestations of pancreatitis: uneven edges of the organ, a change in its shape or the presence of a cyst.
Drug treatment
Medicines used to treat pancreatitis should eliminate acute inflammation and the effects of pathogenic factors.
 In the period of exacerbation, the gland needs functional rest provided by bed rest and sparing fasting: antacids (Almagel or Bourget potion) should be used 5-6 times a day. With exacerbation, Ranitidine and Histodil are prescribed. In case of infection, antibiotics Gentamicin and Ampicillin are recommended.
In the period of exacerbation, the gland needs functional rest provided by bed rest and sparing fasting: antacids (Almagel or Bourget potion) should be used 5-6 times a day. With exacerbation, Ranitidine and Histodil are prescribed. In case of infection, antibiotics Gentamicin and Ampicillin are recommended.
To eliminate the pain, antispasmodics No-Shpa or Papaverin are prescribed, and when they are strengthened, Analgin and Baralgin are found.
Pancreatitis Diet
In addition to taking pills and other forms of medications for pancreatitis, the patient should adhere to a special diet.
To alleviate the symptoms of pathology, the following products should be excluded from the menu:
- products from muffin, dough;
- fish and meat broths;
- fatty, salted meat, fish;
- smoked meats, canned food;
- some types of cereals (barley, corn, millet);
- some vegetables (cabbage, pepper, radish);
- sweets, chocolate, jam;
- carbonated drinks, cocoa, coffee;
- sauces, spices, seasonings.
Allowed to eat foods from the list:
- cereals (except prohibited);
- low-fat fish, meat, cottage cheese;
- soft-boiled eggs;
- steamed puddings;
- butter (up to 30 grams);
- vegetables (except prohibited);
- unsweetened jelly and jelly;
- mineral non-carbonated water, tea.
Recommendations for food regimen in chronic and acute pancreatitis:
- The patient needs to follow the established menu for at least 2 months.
- At least 1.5 liters of liquid should be consumed daily, dividing the intake into 200 ml portions. It is useful to use a rosehip broth, tea.
- In the acute stage, the patient is best left to starve for 1-2 days. However, this procedure should be carried out only after the approval of the doctor. Getting out of fasting is worth it gradually.
- Fat-free protein products should be boiled or steam processed.
- Servings of food should be made small and bring the number of meals up to 5-6 times a day.
- It is best to eat in liquid or semi-liquid form.
Remission of chronic pancreatitis requires compliance with the following recommendations:
- consume more protein foods, reducing the intake of carbohydrates and fats;
- minimize the amount of salt consumed (no more than 6 g per day).
Note! Often the stage of exacerbation occurs if the patient abruptly changes his eating habits. For example, if after some time following the diet begins to abuse products from the prohibited list.
Surgery
Surgical therapy of pancreatitis is recommended if there are a number of indications:
- pancreatic ascites;
- intraductal bleeding;
- stenosis of the duodenum or pancreatic duct;
- pathology not amenable to conservative therapy.
The most common surgical methods for pancreatitis include the following:
- Distal gland resection. It consists in removing the body and tail of the organ. Recommended if the lesion does not capture the gland in full.
- Subtotal resection. It involves the removal of the body, tail and part of the head of the organ. In this case, areas adjacent to the duodenum are preserved. It is indicated for total damage to the gland.
- Necrsecvestrectomy. The existing fluid formation is subject to puncture, after which the ducts are washed.
Operations can be performed under the control of x-rays and ultrasound.
Prevention of new exacerbations
The best prevention of pancreatitis is recognized as the rejection of the frequent use of alcohol and tobacco products.
You should also follow the principles of a healthy diet - minimize the amount of fatty and spicy foods, eat regularly in small portions. The menu should include a sufficient amount of trace elements and vitamins.
At the slightest complaint about a violation of the digestive tract, you should contact a gastroenterologist.
Methods of treating pancreatitis largely depend on the age of the patient, as well as the degree of neglect of the disease. In order to prevent exacerbations and related complications, it is recommended that healthy and already sick pancreatitis people pay careful attention to their lifestyle and diet.
If conservative methods of therapy were powerless, the patient is indicated for surgery.